Military suicides have occurred so often, top commanders are taking notice
By Ashraf Khalil and Lolita C. Baldor, Associated Press
WASHINGTON — After finishing a tour in Afghanistan in 2013, Dionne Williamson felt emotionally numb. More warning signs appeared during several years of subsequent overseas postings.
“It’s like I lost me somewhere,” said Williamson, a Navy lieutenant commander who experienced disorientation, depression, memory loss and chronic exhaustion. “I went to my captain and said, ‘Sir, I need help. Something’s wrong.’”
As the Pentagon seeks to confront spiraling suicide rates in the military ranks, Williamson’s experiences shine a light on the realities for service members seeking mental health support. For most, simply acknowledging their difficulties can be intimidating. What comes next can be frustrating and dispiriting.
In March Defense Secretary Lloyd Austin announced the creation of an independent committee to review the military’s mental health and suicide prevention programs. According to Defense Department data, suicides among active-duty service members increased by more than 40% between 2015 and 2020. The numbers jumped by 15% in 2020 alone.
A 2021 study by the Cost of War Project concluded that since 9/11, four times as many service members and veterans have died by suicide as have perished in combat. The study detailed stress factors particular to military life: “high exposure to mental, physical, moral and sexual trauma, stress and burnout, the influence of the military’s hegemonic masculine culture, continued access to guns and difficulty reintegrating into civilian life.”
Understand the mental health landscape of Colorado each week. Get the Moodfuel Newsletter.
The Pentagon did not respond to repeated requests for comment. However, Austin has publicly acknowledged that the Pentagon’s current mental health offerings, including a Defense Suicide Prevention Office established in 2011, have proven insufficient. “It is imperative that we take care of all our teammates and continue to reinforce that mental health and suicide prevention remain a key priority,” Austin wrote in March. “Clearly we have more work to do.”
Last year the Army issued fresh guidelines to its commanders on how to handle mental health issues in the ranks, complete with briefing slides and a script. Daunting long-term challenges remain. Many soldiers fear the stigma of admitting to mental health issues within the internal military culture of self-sufficiency. Those who seek help often find the stigma not only real, but compounded by bureaucratic obstacles.
Much like the issue of food insecurity in military families, a network of military-adjacent charitable organizations has tried to fill the gaps with programs and outreach efforts. Some are purely recreational, such as an annual fishing tournament in Alaska designed to provide fresh air and socialization for service members. Others are more focused on self-care, like an Armed Services YMCA program that offers free childcare so that military parents can attend therapy sessions.
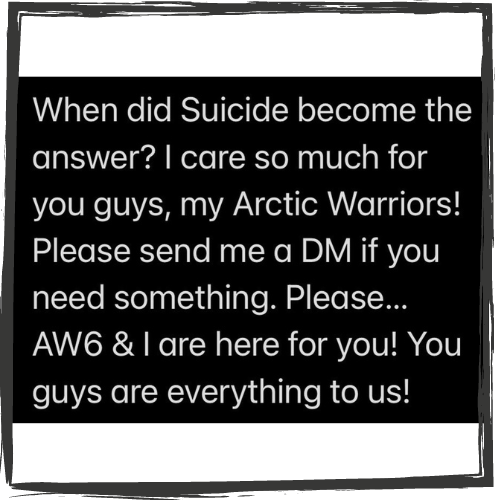
The situation in Alaska is particularly dire. In January, after a string of suicides, Command Sgt. Maj. Phil Blaisdell addressed his soldiers in an emotional Instagram post.
U.S. Sen. Lisa Murkowski, R-Alaska, said that while posting to Alaska can be a dream for some service members, it’s a solitary nightmare for others. “You’ve got to be paying attention to this when you see the statistics jump as they are,” she said. “Right now, you’ve got everybody. You’ve got the Joint Chiefs looking at Alaska and saying, ‘Holy smokes, what’s going on up there?’”
The stresses of a posting can be compounded by a shortage of on-the-ground therapists. Base healthcare workers say they are understaffed, burned out and can’t see patients on a timely basis; soldiers wait weeks for appointments.
“We have people who need our services and we can’t get to them,” one longtime counselor told Army Secretary Christine Wormuth. “We need staff and until we get them, we will continue to have soldiers die.”
Sgt. Antonio Rivera, an 18-year veteran who completed three tours in Iraq and a year at Guantanamo Bay in Cuba, freely acknowledges that he has serious PTSD. “I know that I need help. There’s signs and I’ve waited long enough,” said Rivera, 48, who is assigned to Fort Hood in Texas. “I don’t want my children to suffer because of me not going to get help.”
He’s doing yoga, but says he needs more. He’s reluctant to seek help inside the military. “Personally I’d feel more comfortable being able to talk to someone outside,” he said. “It would allow me to open up a lot more without having to be worried about how it’s going to affect my career.”
Despite the on-base presence of “tons of briefings and brochures on suicide and PTSD,” Williamson said she found herself fighting for years to get time off and therapy. “It’s a wonder how I made it through,” she said.
Eventually, she entered an in-patient program in Arizona. When she returned, a therapist recommended equine-assisted therapy, a breakthrough.
Now Williamson is a regular at the Cloverleaf Equine Center in Clifton, Virginia, where riding sessions can be combined with a variety of therapeutic practices and exercises. Working with horses has long been used as a form of therapy for people with physical or mental disabilities and children diagnosed with autism. In recent years, it has been embraced for helping servicemembers with anxiety and PTSD.
“In order to be able to work with horses, you need to be able to regulate your emotions. They communicate through body language and energy,” said Shelby Morrison, Cloverleaf’s communications director. “They respond to energies around them. They respond to negativity, positivity, anxiety, excitement.” Military clients, Morrison said, come with “a lot of anxiety, depression, PTSD.… We use the horse to get them out of their triggers.”
For Williamson, the regular riding sessions have helped stabilize her. She still struggles, and said her long campaign for treatment has damaged her relationship with multiple superior officers. She’s currently on limited duty and isn’t sure if she’ll retire when she hits her 20-year anniversary in March.
Nevertheless, she says, equine therapy has helped her feel optimistic for the first time in recent memory. “Now even if I can’t get out of bed, I make sure to come here,” she said. “If I didn’t come here, I don’t know where I would even be.”

For service members, veterans and military families interested in Equine Assisted Therapy or Equine-Assisted Psychotherapy, here are some options throughout Colorado:
- Colorado Equine Specialist, Parker
- Holistic Therapeutic Equine Center, Colorado Springs
- Medicine Horse, Boulder
- Colorado Horse Power, Castle Rock
- War Horse Ranch, Steamboat Springs
- Amani Counseling, Ft Collins
- Dream Catcher Therapy Center, Olathe
- Smiling Goat Ranch, Carbondale
- Sunny Horse Foundation, Denver
- Operation Equine, Boulder
- Hearts and Horses, Loveland
- Promise Ranch, Castle Rock
- Full Circle Alliance, Coaldale
- 10th Mountain Equine, Avon
Note: Moodfuel News does not endorse any specific program or facility. This listing is informational only.


